
Therefore, screening and diagnostic test protocols for COVID-19 are still required. Meanwhile, the virus continues to evolve through one or more mutations, which leads to the possibility of ineffectiveness of COVID-19 vaccines. Currently, safe and effective vaccines for controlling the COVID-19 pandemic have been approved and made available by the WHO, including those developed by Pfizer, Moderna, AstraZeneca, Johnson & Johnson, and Sinopharm, which have helped decrease the number of infected patients, severity of symptoms, and rate of mortality. The WHO also declared COVID-19 to be a public health emergency of international concern requiring international cooperation and enforcement of a quarantine policy. COVID-19 has since become a globally recognized pandemic declared by the World Health Organization (WHO) the disease presents as a severe acute respiratory syndrome and causes death. In December 2019, the coronavirus disease 2019 (COVID-19) emerged in Wuhan, China, and spread rapidly through human-to-human transmission.
#Scatter radiation portable#
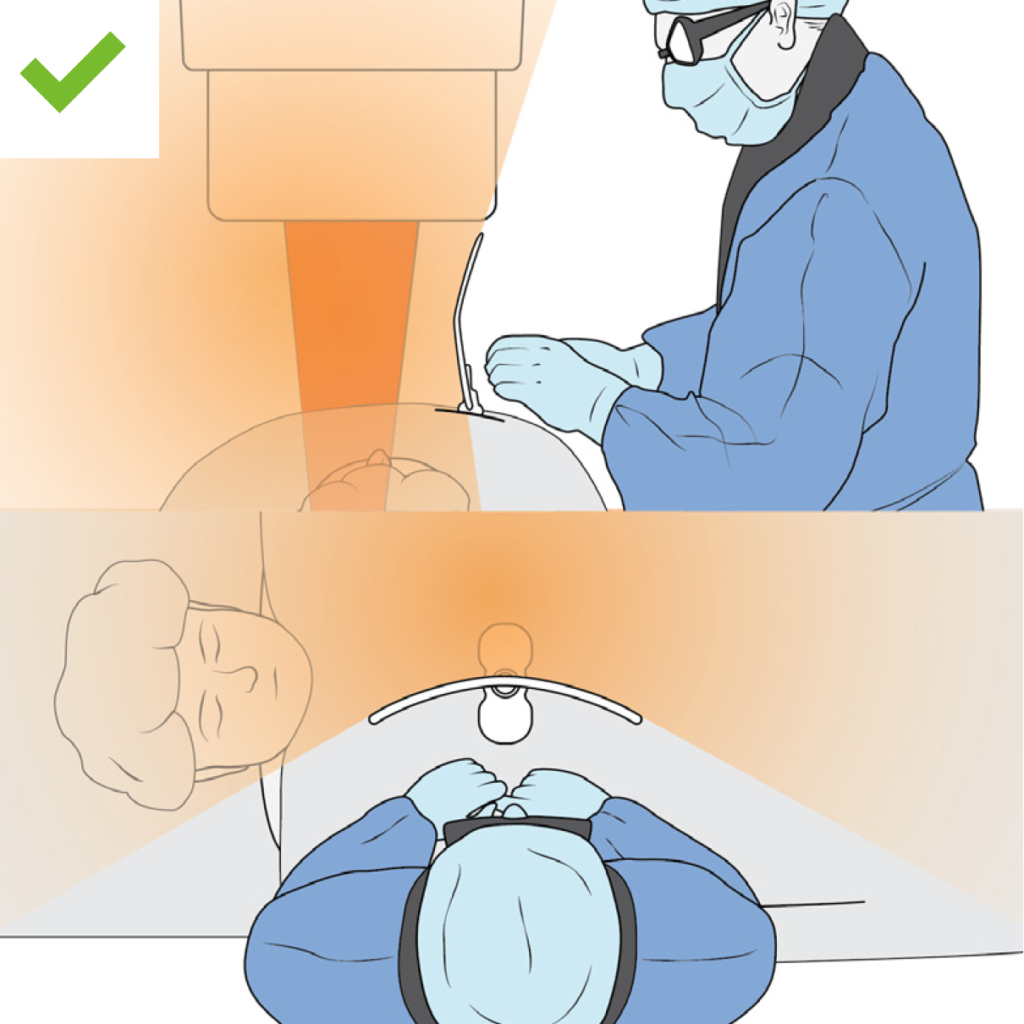
This would allow for an alternative way of performing portable chest radiography for COVID-19 patients without requiring lead shielding.
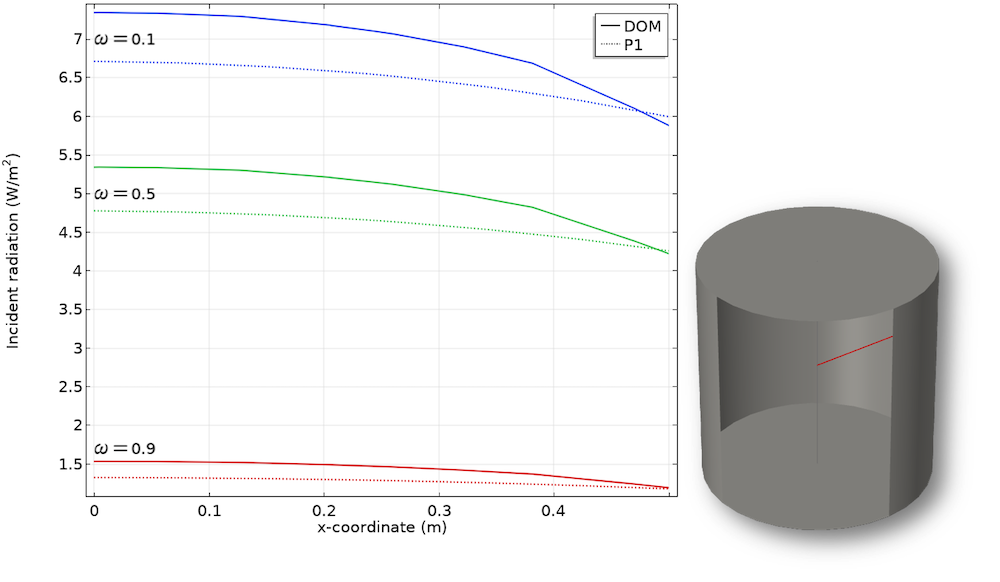
Without lead shielding, RTs must stay at a distance greater than 200 cm from patients for both vertical and horizontal beams to minimize scatter exposure. Correlation analysis between the dosimeter measurement and calculated inverse square law showed good correlation, with an R 2 value of 0.99. Scatter radiation doses of all 40 tests showed a highest and lowest value of 1285.5 nGy at 100 cm in the anteroposterior (AP) semi upright position and 134.7 nGy at 200 cm in the prone position, respectively. Additionally, the doses were compared using the paired t test ( p < 0.005) to determine suitable positions for workers who did not wear lead protection that adhered to radiation safety requirements. The tests were conducted with and without lead shielding. Radiation measurements were performed using the PBU-60 whole body phantom to determine scatter radiation doses at 100–200 cm and eight different angles around the phantom. This study aimed to investigate scatter radiation doses received at various distances, directions, and positions. However, during the pandemic, the use of a lead shield caused a heavy weight burden on workers who were responsible for a large number of patients. Normally, when performing a portable X-ray, radiation protection equipment is critical as it reduces the scatter radiation dose to hospital workers. Radiological technologists (RTs) are often required to perform portable chest X-ray radiography on these patients. The result is still higher patient dose.The COVID-19 pandemic has resulted in a large increase in the number of patients admitted to hospitals. Therefore, the relative number of x-rays that undergo Compton interaction increases.Īlso, fewer x-rays reach the image receptor at low kVp-a phenomenon that is usually compensated for by increasing the mAs.
Three primary factors influence the relative intensity of scatter radiation that reaches the image receptor: kVp, field size, and patient thickness.Īs x-ray energy is increased, the absolute number of Compton interactions decreases, but the number of photoelectric interactions decreases much more rapidly. X-rays of types c and d are called image-forming x-rays. X-rays that arrive at the image receptor are those transmitted through the patient without interacting (c)and those scattered in the patient (d). Others interact with the patient and are absorbed (b). Some x-rays interact with the patient and are scattered away from the image receptor (a). Three primary factors influence the relative intensity of scatter radiation that reaches the image receptor: kVp, field size, and patient thickness. X-rays that exit from the patient are remnant x-rays and those that exit and interact with the image receptor are called image-forming x-rays.Īs scatter radiation increases, the radiograph loses contrast and appears gray and dull. Scatter radiation is a secondary radiation produced when an x- ray interact with the patient and the energy is not enough for an x- ray to reach the IR.


 0 kommentar(er)
0 kommentar(er)
